Protect your family from respiratory illnesses. Schedule your immunization here >

Ranked nationally in pediatric care.
Arkansas Children's provides right-sized care for your child. U.S. News & World Report has ranked Arkansas Children's in seven specialties for 2025-2026.

It's easier than ever to sign up for MyChart.
Sign up online to quickly and easily manage your child's medical information and connect with us whenever you need.

We're focused on improving child health through exceptional patient care, groundbreaking research, continuing education, and outreach and prevention.

When it comes to your child, every emergency is a big deal.
Our ERs are staffed 24/7 with doctors, nurses and staff who know kids best – all trained to deliver right-sized care for your child in a safe environment.

Arkansas Children's provides right-sized care for your child. U.S. News & World Report has ranked Arkansas Children's in seven specialties for 2025-2026.

Looking for resources for your family?
Find health tips, patient stories, and news you can use to champion children.

Support from the comfort of your home.
Our flu resources and education information help parents and families provide effective care at home.

Children are at the center of everything we do.
We are dedicated to caring for children, allowing us to uniquely shape the landscape of pediatric care in Arkansas.

Transforming discovery to care.
Our researchers are driven by their limitless curiosity to discover new and better ways to make these children better today and healthier tomorrow.

We're focused on improving child health through exceptional patient care, groundbreaking research, continuing education, and outreach and prevention.

Then we're looking for you! Work at a place where you can change lives...including your own.

When you give to Arkansas Children's, you help deliver on our promise of a better today and a healthier tomorrow for the children of Arkansas and beyond

Become a volunteer at Arkansas Children's.
The gift of time is one of the most precious gifts you can give. You can make a difference in the life of a sick child.

Join our Grassroots Organization
Support and participate in this advocacy effort on behalf of Arkansas’ youth and our organization.

Learn How We Transform Discovery to Care
Scientific discoveries lead us to new and better ways to care for children.

Learn How We Transform Discovery to Care
Scientific discoveries lead us to new and better ways to care for children.

Learn How We Transform Discovery to Care
Scientific discoveries lead us to new and better ways to care for children.

Learn How We Transform Discovery to Care
Scientific discoveries lead us to new and better ways to care for children.

Learn How We Transform Discovery to Care
Scientific discoveries lead us to new and better ways to care for children.

Learn How We Transform Discovery to Care
Scientific discoveries lead us to new and better ways to care for children.

When you give to Arkansas Children’s, you help deliver on our promise of a better today and a healthier tomorrow for the children of Arkansas and beyond.

Your volunteer efforts are very important to Arkansas Children's. Consider additional ways to help our patients and families.

Join one of our volunteer groups.
There are many ways to get involved to champion children statewide.

Make a positive impact on children through philanthropy.
The generosity of our supporters allows Arkansas Children's to deliver on our promise of making children better today and a healthier tomorrow.

Read and watch heart-warming, inspirational stories from the patients of Arkansas Children’s.

Hello.

Arkansas Children's Hospital
General Information 501-364-1100
Arkansas Children's Northwest
General Information 479-725-6800

Shiloh Robertson: Shining Star for ENT, Endocrinology
A Journey of Hope, Healing and Faith at Arkansas Children's
January 27, 2025

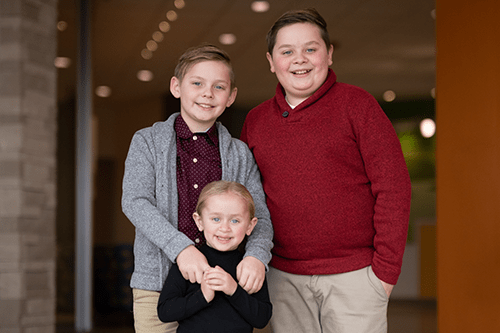
Shiloh Robertson, 4, tilts her head, hands resting below her chin, smiling as her piercing blue eyes stare into the camera inside the Family House room at Arkansas Children's Northwest on Dec. 17. After her photo shoot celebrating her journey to health with Arkansas Children's, she's chatting about a recent trip to Disneyland, proudly sharing about all the princesses she met, clutching her tie-dyed bear in a purple Rapunzel dress.
It’s clear Shiloh is the star of her family, the youngest child of Alan and Heather Robertson, and sister to Whitman, 11, and Harrison, 9.
“She is silly, and she knows she is loved,” her mom said, as her dad admitted, “She knows that the four of us revolve around her.”
And she was always their world — not because she was the baby of the family or the only girl, but because her bright light was so close to burning out.
After struggling to breathe following delivery on Oct. 22, 2020, Shiloh began her years-long journey with Arkansas Children’s, which led to emergency surgery for nasal pyriform aperture stenosis (PAS) and daily growth hormone shots for hypopituitarism.
"God ordained these people to have passions, interests and gifts - this is a blessing from God. I think Arkansas Children's is a blessing from God to this region. I wouldn't have made it without my faith," said Alan, pastor of Calvary Church Lowell. His wife added, "I feel the same way about Arkansas Children's; they were a Godsend. We know God did a miracle."
Flight on Angel One
Before Shiloh was born, Heather felt something was missing. While the couple, married for 14 years, adored their two sons and the baby they lost to miscarriage, Heather knew they were meant to have another child.
Shiloh was born in the evening via an emergency C-section at 37 weeks Oct. 22, 2020, in Rogers. While the couple was overjoyed, the excitement was short-lived.
“Everything that could go wrong went wrong,” her mom explained.
Shiloh was intubated in the neonatal intensive care unit (NICU) at Mercy Hospital Northwest Arkansas in Rogers when air would not pass through her nose. Babies mostly breathe through their noses until about three to four months old.
“I was just standing by the bed in the NICU praying over my daughter and sobbing,” Alan said.
He was soon told his baby girl would be taken to Arkansas Children’s — and not Arkansas Children’s Northwest (ACNW), a short ambulance ride away to Springdale, but airlifted via an Angel One helicopter to Arkansas Children’s Hospital (ACH) in Little Rock. The Angel One Patient Transport System has seven vehicles, including five ground ambulances and two Sikorsky S-76D helicopters. Angel One can reach patients anywhere in the state within 55 minutes. The Angel One transport team brings more than 90% of NICU babies from in-state or out-of-state, with 10% coming from the emergency room or directly from clinics.
By around 4:45 a.m., Alan was boarding Angel One with Shiloh before Heather ever had a chance to meet her.
"The one thing I remember about the pilots from Angel One is that they were calm. They said, 'Sir, it's going to be fine; this is what we're going to do.' In 45 minutes flat, we were at the rooftop at ACH," Alan said. "It struck me how much they cared. They weren't in a rush, and I mean that in a good way. They have this under control."
Life-Saving Surgery
On Oct. 24, Heather’s birthday, she finally met her daughter in the ACH NICU. Andre’ Wineland, M.D., MSCI, FAAP, a pediatric otolaryngologist at Arkansas Children's and associate professor of pediatric otolaryngology head-neck surgery and director of the Pediatric Otolaryngology Fellowship at the University of Arkansas for Medical Sciences (UAMS), told the family Shiloh had a rare deformity called nasal pyriform aperture stenosis (PAS). Nasal passages do not grow wide enough with this condition, causing nasal blockage and affecting one in 25,000 children. It has no known cause.
"Pediatric otolaryngologists receive additional training after residency to learn how to manage children with PAS. Additionally, children with PAS require multidisciplinary care from subspecialty trained physicians and other team members in a dedicated pediatric facility like Arkansas Children's Hospital to provide the best care for children like Shiloh," Dr. Wineland said. "PAS is diagnosed with a CT scan of the face when the opening of the front of the nose is measured at less than 11 millimeters. For reference, a dime is 18 millimeters in width. Two grains of rice placed end to end is 11 millimeters."
In many cases of PAS, a prenatal ultrasound cannot provide the necessary amount of detail to confirm the diagnosis. It is often discovered after birth.
"Dr. Wineland was just a gift. He had an incredibly calming presence," Alan said. "He was confident, but he was not overbearing with it."
Dr. Wineland performed Shiloh's life-saving surgery on Oct. 25, just three days after she was born. Some of her jawbone was drilled down to create wider nose openings for her to breathe.
"Surgery involves using a drill and meticulously removing fractions of millimeters of bone to expand her nasal passages. Too much removal can permanently damage the teeth, ability to transport tears or impact the sinuses. After surgery is complete, the incisions are closed and since the incisions are inside the mouth, there are no visible scars," Dr. Wineland said.
Shiloh’s condition was localized to her nose and the pituitary gland at the base of her brain by the bridge of the nose.
She’d spend the next two and a half weeks in the ACH NICU before going home.
"I'd walk in and see a nurse rocking and singing to her. It was attentiveness; they really love those babies. They're not just another patient," Heather said.
Care Across Arkansas Children's
When Shiloh and her family made it back home to Lowell, about 15 minutes outside of Springdale, they were greeted with expert otolaryngology, also known as ENT, care at ACNW, led by Charles Bower, M.D., a pediatric otolaryngologist at ACNW and professor of otolaryngology head-neck surgery at UAMS.

"I remember meeting Dr. Bower for the first time and thinking, 'This guy is so warm and so friendly and so caring.' He just took his time," Alan said. "That was the first time I felt like a sense of normalcy in her care."
Dr. Bower said he treats roughly one patient every year or two with PAS. She has had dilations, which stretch her nasal passages, and will need at least one more surgery in the future to open her nose further, Dr. Bower said.
"While this condition is quite rare, Shiloh's experience is very typical. It tends to be almost a crisis-level problem early on in life, but as we get the kid's nose open and they breathe better, they become more normal over time," Dr. Bower said. "That first three months is really difficult for the families.
However, her health journey took another turn. Shiloh had difficulty eating and would consistently vomit.
"We measured how good a day was by how many times we had to change our sheets because she would vomit. She would get dehydrated. It felt like every week we were in the ACNW emergency room," Alan said.
In February 2021, at ACH, she had her G-tube placed. Shiloh's brothers, both homeschooled, did everything they could to help make their sister comfortable.
"My brother and I would pray over her and sing little songs. I call her my little miracle munchkin," Harrison said, with Whitman adding, "I would try to help mom and dad out by hanging out with Shiloh."
Life was still far from normal.
Shiloh began seeing the endocrinology team for suspected hypopituitarism, a rare condition — which can be associated with PAS — in which the pituitary gland does not produce enough hormones.
“It is called the master gland because it controls a lot of the other glands in our body, such as the thyroid gland, the adrenal gland, all our puberty, growth hormones and even our water balance,” said Dr. Hamza Nasir, M.D., a pediatric endocrinologist at Arkansas Children’s and a clinical assistant professor at UAMS, who took over Shiloh’s endocrinology care when he joined ACNW in March.
Dr. Nasir said the rarity of hypopituitarism comes from the degree to which the pituitary gland is affected.
"In Shiloh's case, the cells that control the adrenal glands and make our stress hormone cortisol were affected, which can be a life-threatening emergency as it was in her case where the body is just not able to respond to stress. It presents as vomiting for no reason, weight loss, extreme fatigue, dizziness, passing out and low blood pressure," he said. "And, if it's affecting the thyroid gland, then symptoms of thyroid underactivity typically present as fatigue, poor growth, not feeling so well and poor energy."
Following her formal diagnosis after an MRI in the ACNW Emergency Department, Shiloh takes growth hormone shots daily, something she'll take until she's finished growing. She was also diagnosed with hypoadrenalism and hypothyroidism, which will require lifelong medications.
"When we started on the hormone supplements, that's when everything changed. She was so lethargic, taking four to five naps a day. She has a new lease on life," Alan said. "She started gaining weight and it brought such a life and vibrancy to her. It gave us confidence to be parents."
Today, thanks to the multidisciplinary care from Arkansas Children’s, Shiloh has grown in more ways than one.
“We give all glory to God in it, but we couldn’t have done this without such a loving, caring children’s hospital, and we tell people that all the time,” Heather said.
This article was written by the Arkansas Children’s content team and medically reviewed by Andre’ Wineland, M.D., Charles Bower, M.D., and Hamza Nasir, M.D.
Meet the Team
Related Services
-
Angel One Patient Transport System
Contact Angel One dispatch for immediate assistance with transport requests or to consult with pediatric sub-specialists for emergent intensive care need.
-
Ear Nose and Throat (Otolaryngology)
The otolaryngology team at Arkansas Children's provides comprehensive Ear, Nose and Throat care, including treatment for congenital anomalies and plastic and reconstructive surgery.
-
Emergency Departments
Find the locations of Arkansas Children's emergency departments in Little Rock and Springdale, and read answers to frequently asked questions about your child's care in the ER.
-
Endocrinology, Diabetes and Obesity
Learn about the nationally-ranked diabetes and endocrine care provided at Arkansas Children's.
Appointments
New and existing patients can visit our appointment hub for several ways to request an appointment, including online scheduling for many services.
Request an appointment



